Carson Surgical Vascular
It’s something that’s been happening within our bodies every moment since the day we were born–blood flow. The vascular system carries blood throughout the entire body–toes to fingers, brain to every cell inside the body–and if our vessels develop plaque, cholesterol, or blockages, well that’s a serious situation in need of expert care.
Every second of every day your blood vessels carry life sustaining blood from your heart to every part of your body, and then back to your heart again. Diseases that affect your blood vessels can prevent them from doing their job. Keeping those vessels open and flowing properly is essential and requires expert care.
At Carson Surgical Vascular, our vascular surgeons are among the best at deploying a comprehensive array of open, minimally invasive, and hybrid advanced technological options, both in the hospital and in the office, in order to make your blood vessels healthy again.
Dialysis Access
Dialysis could be your lifeline, and it has been just that for over 600,000 kidney disease patients nationwide.
At Carson Surgical Vascular, we create dialysis access for you using your own blood vessels. This will provide you a reliable method for regular hemodialysis. This procedure can be life-changing, and life-saving, for patients suffering from kidney disease.
Ultrasound Lab
When it comes to diagnosing and treating arterial and venous vascular disease, vascular ultrasound is an indispensable tool. Vascular ultrasound essentially uses sound waves to both image blood vessels and to determine how well the blood is flowing through them. It is painless, inexpensive, and non-invasive which is perfect for the long term management of vascular disease. Still, not all facilities that provide ultrasound services are equal. In order to be effective, vascular ultrasound has to be precise and accurate. The results from vascular testing must be able to identify and pinpoint areas of vascular disease to guide medical and surgical management.
The vascular ultrasound lab at Carson Surgical Group is part of a comprehensive vascular program that helps to ensure that we can achieve the best possible outcome for the patients that we manage. Our technical director is Alyssa Hutchinson and she oversees 3 other Registered Vascular Technologists (RVT). All of our ultrasound technologists are specifically trained and board certified in vascular ultrasound. Our medical director, Dr. Kevin D Halow MD, MBA, RVT, FACS, oversees the medical management of the lab. All images are reviewed and finalized by Dr. Halow, and Dr. Shannon H. Beal MD, RPVI, FACS who are both Registered Physicians in Vascular imaging. Finally, our vascular ultrasound lab has been a fully accredited vascular ultrasound lab by the Intersocietal Accreditation Commission (IAC) (https://intersocietal.org/) for over 14 years.
The Vascular Ultrasound Laboratory at Carson Surgical Group provides our patients with state of the art, accurate and precise vascular imaging, to ensure the best possible outcomes. Vascular imaging is what we do.
Varicose Veins
Varicose veins are swollen veins that typically have a blue or dark purple appearance. Oftentimes, the veins are twisted and they’re bulging out from the skin. Varicose veins are usually found in the legs, but they can happen in other parts of your body as well. If you have varicose veins, you might be worried about how they will affect your health. Additionally, they have a significant impact on your appearance. For these reasons, you need to educate yourself on varicose veins causes so that you can determine the course of action for your condition.
Carson Surgical Group’s VNUS Closure procedure is a less invasive alternative to vein stripping. A small catheter is placed in the diseased vein. Then, the use of radio frequency energy is used to close the vein by heating the vein wall and causing contraction of the vein wall which will result in the closing down of the vein.
The VNUS Closure procedure has little or no discomfort associated with it. With over 95% of veins being permanently closed, this procedure has a high degree of success.
Symptoms:
Swollen Limbs
Heaviness and Fatigue
Skin Changes and Ulcers
Pain
Tired, Achy Legs
Vascular and Endovascular Surgery
Peripheral Vascular Disease
Our hybrid operating room is a standard surgical theatre equipped with advanced medical imaging devices that would normally be used in a cardiac catheterization laboratory. Our advanced equipment includes a movable image intensifier (C-Arm used for taking X-rays), a movable gantry (operating table that can be used for X-ray fluoroscopy), a power injector for injecting contrast, and monitors and support systems that allow for complex X-ray imaging. This hybrid operating room has revolutionized the treatment of vascular disease.
This hybrid operating room is a powerful new tool for our management of patients with vascular disease. Because it has all of the capabilities of a standard operating room, nearly any open vascular surgery case can be performed, plus, with the addition of advanced X-ray imaging, as well as other tools such as intravascular ultrasound, the Carson Surgical team can perform complex vascular repairs and reconstructions with minimally invasive methods that were never before possible.
Once the aneurysm is repaired, patients are placed into a surveillance program to monitor the repair. It is very important to maintain ultrasound follow up of the repair. Occasionally, these grafts do require some maintenance. If identified early through continued surveillance, maintenance can usually be done endovascularly as a quick outpatient procedure.
Peripheral Vascular Disease
Peripheral Vascular Disease is a term used to describe diseases affecting the arteries. The arteries are large muscular tubes that carry blood pumped from the heart throughout the body. Arteries have three layers, and it is the middle layer (Tunica Media) that is directly affected in peripheral vascular disease.
Peripheral vascular disease can result in blockages in the arteries or abnormal enlargements of arteries (aneurysms). The risk factors for peripheral vascular disease include a family history of the disease, heart disease, aneurysm disease (genetic component), history of known peripheral vascular disease, smoking, and hypertension. Artery blockages can occur anywhere, but are most commonly found in the lower extremities and in the carotid arteries (the arteries in the neck that take blood to the brain). In each of these areas, there is a unique set of symptoms that occur.
Advances in technology have given the vascular surgeons at Carson Surgical Group a large compendium of techniques to fix these problems, many of which are minimally invasive.
Lower Extremity Peripheral Vascular Disease
When artery blockages occur in the lower extremities, blood flow is restricted to those areas causing immediate harm. As plaque builds up in the artery, the flow of oxygen and nutrients to the extremities is limited. At rest, it may not be a problem, but when the patient begins to walk, the muscles cannot get enough oxygen, which results in lactic acid build up in the muscles and the patient experiences calf cramps that prevents them from walking further.
Resting for a minute allows the lactic acid to be flushed out as the oxygen supply builds back up. The patient can then go on to walk again, but only to be stopped at the same distance again from the cramps in the calf.
In many patients, these blockages are so severe that the tissues in the lower extremities don’t even have enough oxygen at rest. This results in tissue break down, wounds, and pain at rest. This becomes an emergency; unless blood flow is restored, the patient will require an amputation.
Advances in technology now give the vascular surgeons at Carson Surgical Group many different options for repairing artery blockages due to peripheral vascular disease. Most often, patients can be treated with angioplasty (using a balloon to open up the artery) or stenting (putting a spring in the artery to keep it open). Other options include manually cleaning out the artery (called endarterectomy) or with a surgical bypass around the blockage.
Once the artery is fixed, patients are monitored using our advanced ultrasound surveillance. All patients with vascular disease must be followed with ultrasound.
It’s important to note, fixing an artery in a patient with peripheral vascular disease does not cure the disease, but fixes the affected artery. Peripheral vascular disease will progress over time and re-intervention may be required. Re-intervention is easier if found early rather than waiting for the symptoms to recur.
Carotid Artery Disease
Carotid arteries are the dominant arteries that carry blood from the heart to the brain, located in the front of the neck on both sides. Risk factors for carotid arteries are the same as those for peripheral vascular disease.
Blockages in the carotid artery can result in a stroke, and unfortunately, carotid artery blockages are often silent until the first stroke event occurs. Symptoms of a stroke include:
Facial droop
Inability to speak or understand
Blindness in one eye
Loss of function of an arm or leg or both
Screening for carotid artery disease is extremely important as by the time that symptoms occur, it may be too late. This screening for carotid artery disease is done with ultrasound in our Ultrasound Lab.
Repairing A Blocked Carotid Artery
Repairing a blockage in the carotid artery is most often done with an endarterectomy, where the artery is cleaned out using an open surgical approach. While there are other methods available, such as stenting, carotid endarterectomy remains the standard of care.
As with peripheral vascular disease treatment in the lower extremities, vascular disease in the carotid arteries must be followed with ultrasound in our Ultrasounds Lab after treatment. Plaque can recur and re-intervention may be required in order to prevent a stroke.
Aneurysm Disease
An aneurysm is an abnormal enlargement of an artery. Nearly any artery can develop into an aneurysm, something analogous to blowing up a balloon. The larger the balloon gets the easier it is to blow up; eventually rupturing if it gets large enough.
While the risk for most aneurysms is the risk of rupture, aneurysms can also develop so much clot inside them that they completely block off the artery, resulting in a sudden lack of blood flow to any structure down-stream of the blocked artery. Usually this occurs in the popliteal arteries (the arteries behind the knees).
Aneurysms are silent (they do not cause any symptoms), so the only way to know if you have an aneurysm is to scan in our Ultrasound Lab.
Risk factors for aneurysms include:
A family history of aneurysm disease (genetic component)
History of known peripheral vascular disease
Smoking
Hypertension
If you have any of the risk factors for aneurysm disease, you should consider being screened in our Ultrasound Lab by the age 65.
Treat or Prevent Vascular Disease
Hemodialysis Access
What is Dialysis?
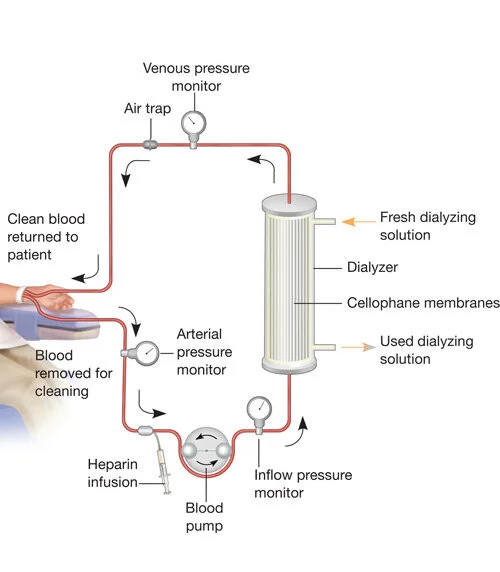
Your kidneys remove waste from your blood, but when your kidneys fail, they can no longer do this important work. One way to remove that waste with failed kidneys is to use hemodialysis. “Heme” meaning ”blood” and “dialysis” referring to the process where particles in a liquid are separated on the basis of differences in their ability to pass through a membrane, this is hemodialysis.
Hemodialysis cleans your blood by taking it out of your body, passing it through a machine that has a membrane that takes out the waste products, and then puts it back into your body.
Your kidneys remove waste from your blood, but when your kidneys fail, they can no longer do this important work. One way to remove that waste with failed kidneys is to use hemodialysis. “Heme” meaning ”blood” and “dialysis” referring to the process where particles in a liquid are separated on the basis of differences in their ability to pass through a membrane, this is hemodialysis.
Hemodialysis cleans your blood by taking it out of your body, passing it through a machine that has a membrane that takes out the waste products, and then puts it back into your body.
How Can Vascular Surgery Help You Get Dialysis?
In order to be able to do hemodialysis, blood must be taken from your body and put back. In order to do this and perform dialysis, we need to be able to circulate 500 cc (2 cups) per minute of blood through the dialysis machine.
The arteries are the thick muscular tubes that carry blood from the heart out to the body, while the veins are the thin walled vessels that carry blood back from the body to the heart. What some don’t know is that the heart does not pump blood back, it only pumps it out and the blood must get back on its own–that’s the job of the arteries.
Arteries have more than enough blood flow to allow for dialysis, however, you cannot stick a needle into an artery over and over again–it will damage the artery. You can stick a needle into a vein over and over again and it will not damage it, but unfortunately, there isn’t enough blood coming back through the veins to run through a dialysis machine. The solution? Here at Carson Surgical Group, we connect the artery to the vein and “borrow” some blood flow from the arteries–Dialysis Access. Once this is done, we can stick the vein over and over again and borrow the added blood to run through the dialysis machine. This all allows for an end result of clean blood and waste products removed.
Creating Dialysis Access
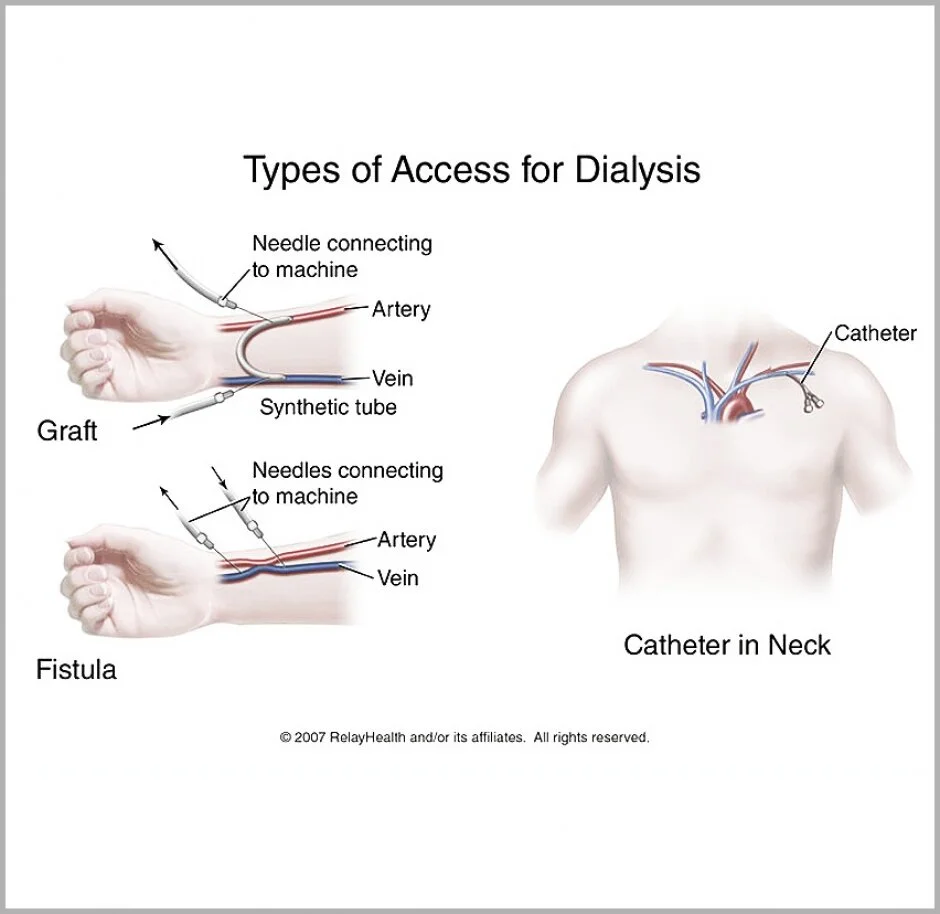
There are two Dialysis Access options, a fistula or a graft.
A fistula is made by connecting an artery to a nearby vein. Blood flows into the vein and causes the vein to enlarge. It’s common that fistulas need weeks or even months to develop before they’re ready. Fistulas are our best option as they last longer and do not get infected. If at all possible, we create a fistula.
A graft may be sewn between an artery and a vein if a fistula is not an option. With a graft, blood flows through the graft from the artery to the vein. A graft is usually ready to use in a few weeks, but may not last as long as a fistula in the long run. We use grafts only if a fistula cannot be created.
Caring For Your Access & Feeling the “Thrill”
To help your access stay clean, healthy, and last, follow these simple guidelines:
Don’t wear tight clothing or jewelry near and around your access.
Don’t let anyone take your blood pressure on or draw blood from the arm with the access.
Protect your access from being hit or cut.
Wash your hands often and keep the area around your access clean.
If you put your fingers over your access, you should feel the blood rushing through it, this is called a thrill. Feel your thrill as often as you are told, usually once or twice a day. If you can’t feel it, tell your healthcare provider right away. Blood may not be flowing through your access the way it should.
Other problems you should alert your doctor can include:
Pain or numbness in your hand or arm
Bleeding, redness, or warmth around your access
Your access is suddenly bulging out more than usual
If you have a fever over 101ºF